What is a Lucentis biosimilar?
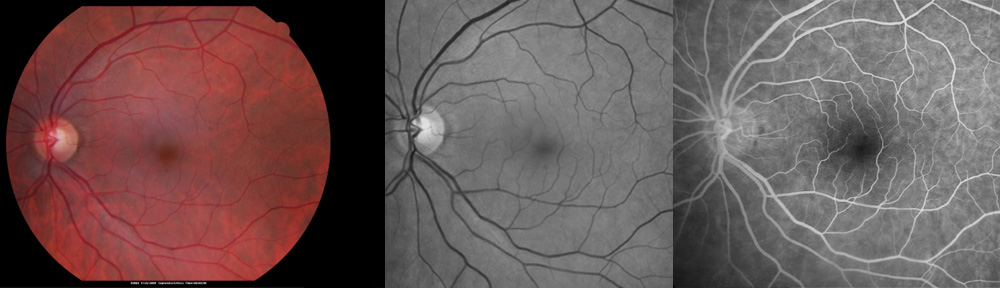
Lucentis is a medication used in the treatment of a variety of conditions including wet-type macular degeneration, diabetic retinopathy, and retinal vein occlusion. Lucentis biosimilars are less-expensive medications manufactured to work in a fashion similar to Lucentis. It is important to remember that Lucentis biosimilars are not identical medications to Lucentis. In the US, Lucentis biosimilars include Byooviz and Cimerli.
How effective are Lucentis biosimilars?
Lucentis was proven in extensive studies to be very effective. In wet-type macular degeneration, a large study showed that monthly injections of Lucentis over a two-year period offered a 90% chance of stable or improved vision. Similar benefits are seen in other retinal conditions as well. The biosimilars were approved for use by the FDA as they appear to be non-inferior. Further research will reveal more details.
What are the risks of Lucentis biosimilars?
Severe complications are very rare, but risks of Lucentis injection include bleeding, infection, inflammation, retinal detachment, glaucoma, cataract, and loss of vision. There may be a small increased risk (1%) of stroke or heart attack with Lucentis. The risk of stroke may be related to concurrent illness and the older age of patients in which these medications are used. Pregnancy should be avoided while on Lucentis therapy. All of these risks apply to biosimilars, as well. Furthermore, the question of whether biosimilars pose additional (or less) risk will be determined over time.
Why change from Lucentis to a biosimilar medication?
Usually an insurance company prompts the need to change from Lucentis to a biosimilar medication to lower their costs. This may be a disadvantage to signing up for a Medicare Advantage insurance plan. When a doctor must change from Lucentis to a biosimilar, he may need to take precautions in order to reduce the risk of problems. For example, he may initially inject Byooviz or Cimerli at 4-week intervals before attempting to extend the treatment interval in order to assure effectiveness. He may monitor the patient more closely to identify inflammation or high eye pressure. After injection, patients should report any new symptoms without delay.
Are doctors given financial incentives to prescribe Cimerli and Byooviz?
Manufacturers of new medications often provide incentives in the form of rebates to doctors. To determine if your doctor receives large payments from drug companies, visit the CMS website and enter your doctor’s name in the search box. I take great pride in advocating for my patients in the selection of medications, rather than pander to the drug companies.
For a telemedicine consultation with Dr Pautler, please send email request to spautler@rvaf.com. We accept Medicare and most insurances in Florida. Please include contact information (including phone number) in the email. We are unable to provide consultation for those living outside the state of Florida with the exception of limited one-time consultations with residents of the following states: Alabama, Arkansas, Connecticut, Georgia, Minnesota, and Washington.
Copyright ©2023 Designs Unlimited of Florida. All Rights Reserved.