How does tobacco affect the eyes?
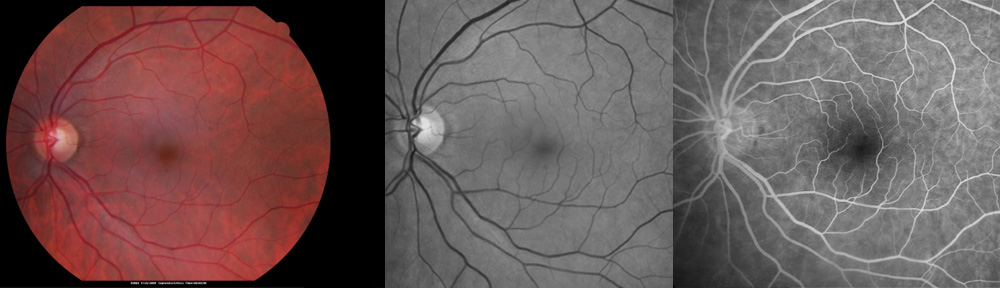
Tobacco use is widely known to cause lung damage, but the eyes are also affected. Bothersome irritation of the eyes is caused by smoke from tobacco especially in patients with dry eyes. However, permanent loss of vision may occur from such problems as macular degeneration, retinal vein occlusion, ocular histoplasmosis syndrome, glaucoma, cataract, Grave’s Disease (a thyroid condition that affects the eyes), uveitis (inflammation of the eye), ischemic optic neuropathy, and diabetic retinopathy. Tobacco appears to play a role in causing and/or worsening these conditions. Tobacco is known to promote hardening of the arteries, and this may harm blood flow to the eye. Tobacco also promotes the development of blood clots, which may block blood flow in the eye. Tissue damage also occurs from toxic compounds in tobacco that cause a chemical reaction called oxidation. More research is needed to fully understand the role of tobacco in causing loss of vision.
What resources are available to help stop tobacco use?
Because most people cannot stop tobacco “cold turkey,” many resources are available to help quit the habit. Counseling may provide much needed support in the process of stopping tobacco use. For free classes and one-month’s supply of nicotine replacement therapy, your doctor can refer you to the Area Health Education Center. Alternatively, you may call 1-877-848-6696. The class schedule may be viewed at www.ahectobacco.com/calendar. If you are interested in talking to informed support staff, please call 1-800-QUIT-NOW. Nicotine replacement therapy plays an important role and several preparations are available over-the-counter. These non-prescription forms of nicotine include gum, lozenges, and patches. Medicare and most insurance companies now cover the costs of prescription medications to help stop tobacco use. These include nicotine nasal sprays, nicotine inhalers, as well as pills (Zyban and Chantix). With the help of counseling, nicotine replacement, and prescription medication, you can live a longer and healthier life without tobacco. For more information please visit www.smokefree.gov.
For a telemedicine consultation with Dr Pautler, please send email request to spautler@rvaf.com. We accept Medicare and most insurances in Florida. Please include contact information (including phone number) in the email. We are unable to provide consultation for those living outside the state of Florida with the exception of limited one-time consultations with residents of the following states: Alabama, Arkansas, Connecticut, Georgia, Minnesota, and Washington.
Copyright © 2013-2022 Designs Unlimited of Florida. All Rights Reserved.